There is no exact estimate of how many people we have a piercing within the oral cavity, but according to a 2012 study we are talking about 5.2% of the world population, the consequences on oral health could be many, but recently there has been much attention to the correlation between oral piercing and dental implant health and the periodontium.
Complicanze associate ai piercing
Over time, several oral health complications have been identified due to the presence of oral piercings, among which the most obvious are:
- tongue trauma
- trauma to oral tissues
- infections
- edema
- paresthesias
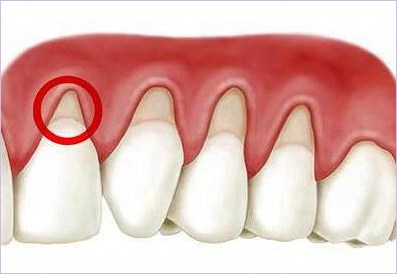
Tongue piercing has also been associated with soft tissue inflammation, a condition that in turn leads to increased plaque buildup, gum bleeding, attachment loss, and marginal bone loss around the teeth.
Piercing and health status of the dental implant and periodontium
In a recent study, published in the International Journal of Dental Hygiene, the influence of tongue piercing on periodontal and peri-implant health status in adults was evaluated.
The sample used for the research included patients with and without tongue piercings, divided into two groups. A questionnaire was used to collect information on gender, age, tongue piercing duration and the presence of implants in operation and their position in the arch, the motivation for wanting to get the piercing, the state of oral hygiene and piercing cleaning habits.
The following parameters were recorded and evaluated:
- plaque index
- gingival index
- clinical attachment loss
- periodontal probing depth
- bone loss
Data were also collected on the type of piercing material, whether plastic or metal, and on their closure, whether ball-shaped or other type.
Peri-implatitis, periodontitis and tongue piercing
The study revealed the following information:
48 (15 male and 33 female) and 49 (19 male and 30 female) subjects were included in the test and control groups.
23 and 25 patients wore ball piercings made of stainless steel and bioplastic, respectively, for an average duration of five years. All individuals in the test group reported removing and cleaning their piercings.
22 patients in the control group and none in the test group were aware of possible oral complications associated with tongue piercing. The most common reason reported for choosing to get a tongue piercing was “it looks classy” and was reported by 25 individuals.
14 did not give any reason why they decided to get tongue piercings and two women reported that the tongue piercing “reflected bravery”.
Twice-daily tooth brushing was reported by 39.6% and 53.1% of individuals in the test and control groups, respectively. Flossing at least once a week was reported by 32.7% of people in the control group. None of the individuals in the test group reported flossing.
In the test group, peri-implant inflammation and bone loss were found to be significantly higher in the anterior mandible than in other parts of the jaw. There was no difference in the control group.
From the data of this study, which must be confirmed in other similar works, it can be concluded that tongue piercing can increase the risk of periodontitis and peri-implant diseases, especially in the anterior mandibular area.
















